Timisoara_Med , 2024(2), 8; doi:10.35995/tmj20240208
Article
Influence of Silver Nanoparticle Integration on the Composition and Surface Properties of Acrylic Dental Resins Employed in Temporary Bridges
1
Department of Oral Implantology, Removable Dentures and Technology, Faculty of Dental Medicine, “Grigore T. Popa” University of Medicine and Pharmacy, 700115 Iași, Romania; ioana.martu@umfiasi.ro (I.M.); antonela.diaconu@umfiasi.ro (D.A.D.P.); giorgio.nichitean@umfiasi.ro (M.G.N.)
2
Department of Surgery, Discipline of Pediatric Dentistry, Faculty of Dental Medicine, “Grigore T. Popa” University of Medicine and Pharmacy, 700115 Iasi, Romania
3
Department of Toxicology, Faculty of Pharmacy, “Grigore T. Popa” University of Medicine and Pharmacy, 700115 Iasi, Romania; jitareanu.alexandra@umft.iasi.ro
4
Department of Periodontology, Discipline of Periodontology, Faculty of Dental Medicine, “Grigore T. Popa” University of Medicine and Pharmacy, 700115 Iasi, Romania; liliana.pasarin@umfiasi.ro
5
Department of Surgery, Discipline of Basics of Physics and Biophysics in Dental Medicine, Faculty of Dental Medicine, “Grigore T. Popa” University of Medicine and Pharmacy, 700115 Iași, Romania; oana.maria.butnaru@umfiasi.ro
6
Department of Prostheses Technology and Dental Materials, Faculty of Dental Medicine, “Victor Babeș” University of Medicine and Pharmacy, 300040 Timișoara, Romania; emanuela.craciunescu@umft.ro
*
Correspondence: carmen.savin@umfiasi.ro; Tel.: +40-723390363
How to cite: Mârțu, I.; Savin, C.; Diaconu-Popa, D.A.; Jităreanu, A.; Nichitean, M.G.; Păsărin, L.; Butnaru, O.M.; Crăciunescu, E. Influence of Silver Nanoparticle Integration on the Composition and Surface Properties of Acrylic Dental Resins Employed in Temporary Bridges. Timisoara Med. 2024, 2024 (2), 8; doi:10.35995/tmj202402038.
Received: 30 April 2024 / Accepted: 12 August 2024 / Published: 30 September 2024
Abstract
:(1) Background: Recognized widely for its irreversible effects, periodontal disease is one of the most prevalent conditions, particularly emphasizing the potential for permanent damage caused by gingivitis, extending to encompass the entirety of the supportive complex, including the connective tissue and alveolar bone. Patients necessitating comprehensive periodontal and prosthetic treatments require an interdisciplinary approach, involving the coordination of pre-treatment procedures and appropriate prosthetic strategies. The adoption of advanced materials and techniques can prove beneficial in addressing complex dental issues. (2) Methods: Forty specimens were prepared using the prescribed procedure, with 20 acting as controls and the other 20 integrating AgNPs. The initial step involved crafting wax patterns of distinct shapes: dumbbell shapes for tensile testing and rectangular shapes for roughness assessments. These dimensions were aligned with ASTM D-638 and ISO 527-2 standards and adjusted to match the specifications of the analysis device for mechanical properties. (3) Results: In this case, the results indicate minimal differences in heat-curing acrylic resins compared to the control samples at a 5% concentration. However, notable disparities arise at concentrations of 10% and 20%. (4) Conclusions: Temporary prosthetic constructions are essential for preventing functional imbalances and complications. Incorporating AgNPs at a 5% concentration maintains mechanical properties while providing antibacterial effects for long-term interim prosthodontic restorations. Higher nanoparticle concentrations may reduce resin mechanical properties without affecting material surface conditions.
Keywords:
periodontal disease; silver nanoparticles; acrylic dental resins; temporary bridgesIntroduction
Periodontal conditions are widely acknowledged as being among the most prevalent, given their irreversible consequences, especially concerning gingivitis, which may result in permanent damage affecting the entire supportive structure, encompassing connective tissue and alveolar bone. Patients requiring comprehensive periodontal and prosthetic treatments necessitate an interdisciplinary approach, involving the coordination of pre-treatment procedures and appropriate prosthetic strategies. Furthermore, the utilization of advanced materials and techniques can prove beneficial in addressing complex dental issues.
Any prosthetic construction must be performed following periodontal treatment, ensuring the healing or stabilization of the affected structures. Therefore, prior to the final prosthetic treatment, provisional prostheses are necessary to allow the patient to maintain the functions of the stomato-gnathic system.
The objective of using temporary restorations includes safeguarding the pulp and periodontal tissues, facilitating guided tissue regeneration, effectively addressing emergency situations, and assessing hygiene protocols, among various other aims. Moreover, such restorations allow for the evaluation of an appropriate occlusal scheme and determined maxillo-mandibular relationships [1]. When selecting materials for provisional restorations, it is crucial to take into consideration their physical, mechanical, and handling characteristics, ensuring that the chosen material fulfills the unique demands of each clinical scenario [2,3].
An important factor to consider is the compatibility of a material with soft tissues and its ability to withstand biological reactions [4]. Furthermore, it is vital to recognize the various demands of interim restorations, including maintaining tooth position stability, which requires marginal precision, structural strength, resistance to wear, and adherence to esthetic standards, while preserving polish and luster [5,6,7].
Temporary prostheses serve as a pivotal phase in anticipating final restorations, facilitating the rehabilitation of abutment health and promoting healing in prosthetic areas and periodontal tissues [8,9]. Traditional materials for provisional restorations can be divided based on their chemical composition: those utilizing mono-meth-acrylates or acrylic resins, including poly-methyl-methacrylate (PMMA) and poly-ethyl/butyl methacrylate (PEMA), and those utilizing di-meth-acrylates or bis-acryl/composite resins, such as bis-phenol A-glycidyl di-methacrylate (Bis-GMA) and urethane di-methacrylate (UDMA). However, these materials, employed in conventional techniques, may exhibit several drawbacks, including low mechanical strength, color instability, and the presence of residual monomers [10,11,12,13].
For several decades, poly-methyl meth-acrylates have been regarded as the standard material of choice. Their benefits include affordability, excellent strength, easy processing and polishing, color stability, and easy of repair. However, these materials also have drawbacks, such as their tendency to generate high exothermic reactions, which can potentially harm the pulp and the release of residual monomers, leading to tissue damage and an allergic sensitivity incidence of 20%, relatively high polymerization shrinkage, unpleasant odor, and potential inconsistencies when manually mixing powder and liquid [14,15].
The incorporation of antimicrobial properties into dental materials has been a significant concern in dentistry, with their efficacy demonstrated in various applications such as orthodontic adhesives, dental instruments, endodontic filling materials, and prosthodontics. Despite ongoing advancements in material science, acrylic resins remain the most commonly utilized material for temporary bridges in prosthodontics.
The antimicrobial effect of AgNPs has been directly correlated with concentration and inversely with particle size. Typically, higher concentrations exhibit greater antimicrobial activity, whereas smaller particles can achieve bacterial eradication at lower concentrations. Particles exceeding 100 nm demonstrate only bacteriostatic properties, whereas smaller particles exhibit bactericidal effects. The antimicrobial efficacy increases with decreasing particle size (<10 nm) due to enhanced penetration into bacteria rather than mere surface interaction. Silver particles have been integrated into acrylic resin to enhance its biological tolerance. Micrometer-sized particles were utilized to enhance resin characteristics, but they posed various limitations. With advancements in nanotechnology and the advantages offered by adding silver nanoparticles to acrylic resins, such as improved processing and smoother surfaces compared to micrometer-sized silver powder, the utilization of silver nanoparticles is favored. Among the available nano-fillers, silver nanoparticles are the most commonly employed due to their ductility, electrical and thermal conductivity, and antimicrobial properties [16]. However, concerns regarding resin discoloration and cost may constrain their usage [17].
This study was conducted to assess the impact of incorporating silver nanoparticles (AgNPs) at concentrations of 5, 10, and 20% on acrylic resin parameters.
Materials and Methods
A total of 40 samples were fabricated using the conventional method, employing the heat-curing acrylic resin Superpont C + B (SpofaDental, Jicin, Czech Republic); 20 samples served as controls, while the remaining 20 incorporated AgNPs.
The initial stage involved creating two distinct shapes of wax patterns: for the tensile tests, the wax patterns were 2 mm thick and fashioned into dumbbell shapes with dimensions of 75 mm in length, 12.5 mm in width at the extremities, and 4 mm in the central region. For the roughness assessments, rectangular wax patterns of the same thickness (2 mm) were utilized, measuring 70 mm in length and 30 mm in width. The chosen dimensions were in accordance with ASTM D-638 and ISO 527-2 standards, and they were adjusted to meet the specifications of the device utilized for analyzing the mechanical properties.
For the surface analysis, the sample sizes were selected in accordance with the specifications outlined by the roughness tester utilized in the study.
Pink wax, 2 mm thick (DistriWax-DinstridentPlus, Suceava, Romania), was employed to realize the wax patterns, which were subsequently transformed into acrylic specimens using the same methodology used for temporary acrylic dental bridges. Initially, the wax patterns were invested in dental stone (Elite Rock class IV gypsum, Zhermack, Badia Polesine, Italy) to create molds. Following mold isolation with a separating agent (Isodent/SpofaDental, Jicin, Czech Republic), the acrylic resin was prepared according to the manufacturer’s instructions: mixing 2 g of powder with 1 g of liquid (or in volume units, 3 parts powder to 1 part liquid), with a mixing time of 1.5 min.
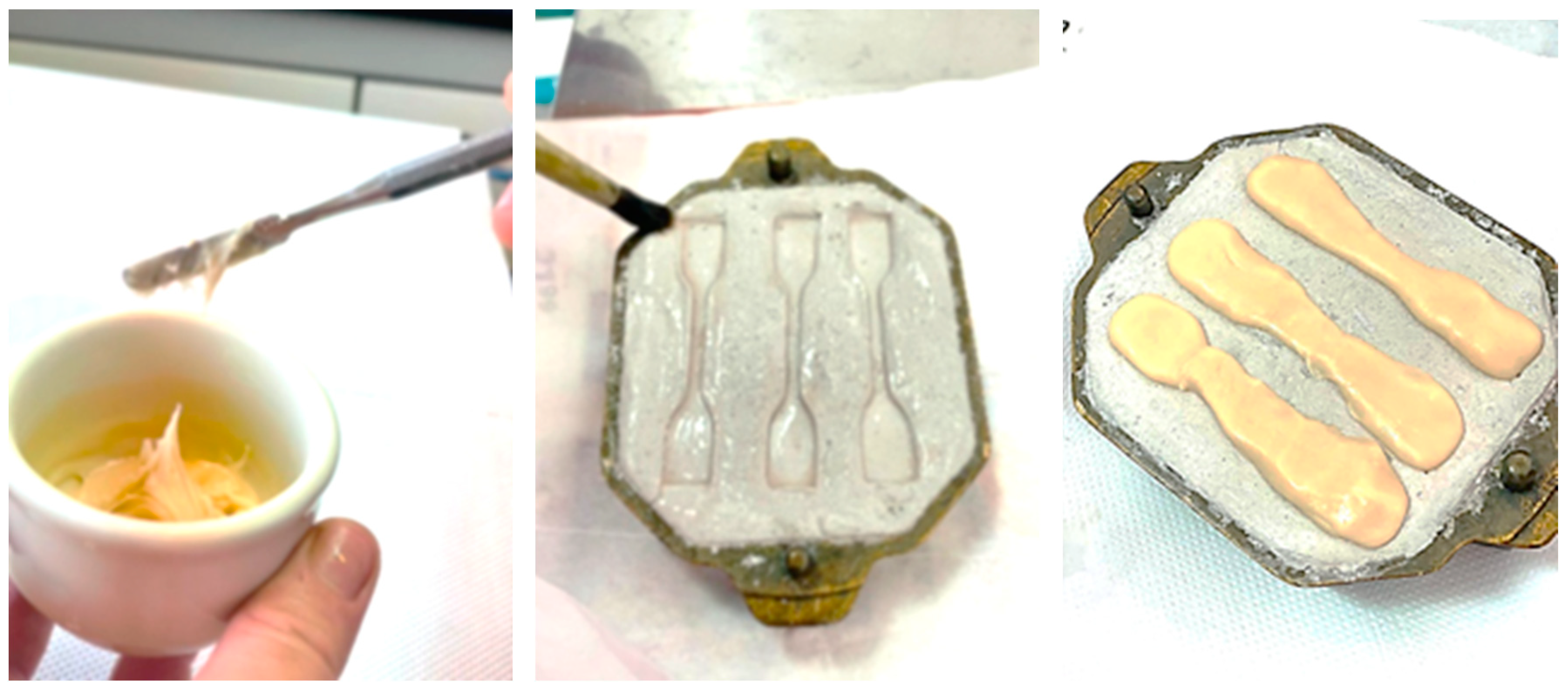
The AgNp in colloidal solution was added to the monomer of acrylic resin by volume proportion in 5, 10, and 20% concentration, except for the control group specimens. The powder and liquid with nanoparticle solution were mixed into a porcelain jar and then the acrylic resin paste and, when the resin had a plastic consistency, it was introduced into the mold and pressed with the help of a hydraulic press. The curing process was performed in a polymerization chamber at a temperature of 100 °C, pressure 2–4 bar, for 40 min [18] (Figure 1).
Figure 1.
Sample realization.
The technological procedures closely resemble those delineated in the protocol for fabricating interim bridges utilizing heat-cured resin within dental laboratory environments. Subsequent to the cooling phase, the specimens were extracted from the mold, subjected to verification, and underwent sandblasting (Figure 2).
Figure 2.
Divesting resin samples.

Following a standardized protocol for finishing and polishing temporary bridges, all samples underwent processing on a single surface utilizing the Acrylic Contouring & Finishing Kit HP (Shofu Dental GmbH, Ratingen, Germany). Initially, the surfaces were adjusted using a dark gray AcryPoint Coarse Grit BP1 tool, mounted in a hand-piece and operated at low speed (10,000 rpm). Subsequently, the finishing touches were applied using a brown AcryPoint Medium Grit BP1 tool (10,000 rpm). To conduct the polishing process, a fine AcryPoints tool (light gray) operating at 5000 rpm and a soft Circular Goat Hair Brush (90 mm diameter) reaching a maximum speed of 4000 rpm were employed. Subsequently, a buffing wheel and universal polishing paste (Ivoclar Vivadent AG, Schaan, Liechtenstein) were employed at 4000 rpm to attain the final gloss.
Tensile testing was performed under ambient conditions in accordance with the ISO 527-1:2000 standard. This involved employing a computer-controlled testing apparatus (Instron 3382) outfitted with a dynamic clip-on strain gauge extensometer (Instron 2620-601) for direct strain measurement. The rectangular specimens were firmly positioned and clamped between the grips of the testing apparatus (Figure 3).
Figure 3.
Instron testing machine.

Tensile loading was applied at a crosshead speed of 1 mm/min. Parameters including Young’s modulus (determined as the slope of a secant line between 0.05% and 0.25% strain on a stress–strain plot), tensile yield (representing the tensile stress at yield), and tensile strength (indicating the maximum tensile stress achieved during the test) were determined. To evaluate surface roughness, measurements were taken for each sample using the Ra and Rz parameters. Ra signifies the arithmetic mean of the absolute values of profile deviations from the mean line of roughness, whereas Rz denotes the average of all values representing the maximum height between the highest and lowest points of the profile within the assessment length for each sample’s roughness profile. Three roughness measurements were taken on the surface of each sample using a Form Talysurf roughness tester (Taylor Hobson, Leicester, England), equipped with a cantilever peak radius with r = 2 μm, and the data were recorded accordingly (Figure 4).
Figure 4.
Form Talysurf roughness tester.

Results
Young’s modulus (E) is a measure of tensile elasticity, derived from Hooke’s law, E = σ / ε, where σ represents stress and ε signifies deformation. It characterizes an object’s propensity to deform along an axis under opposing forces applied along that axis, expressed as the ratio of tensile stress to tensile strain. A reduction in Young’s modulus at a consistent pressure denotes increased deformation, with lower Young’s modulus values suggesting heightened material flexibility. However, excessive flexibility may prove disadvantageous for total prostheses.
The findings reveal that heat-curing acrylic resins demonstrate marginal disparities in comparison to control samples at a 5% concentration, yet they exhibit notable discrepancies at concentrations of 10% and 20% (Figure 5).
Figure 5.
The Young’s modulus calculation of analyzed samples.

Under the influence of pressure, the resin samples undergo initial elastic deformation, marked by reversible elongation. Persistent force application induces plastic deformation, which is irreversible and ultimately leads to fracture. The threshold pressure at which fracture occurs is determined by the mechanical characteristics of the material.
The samples exhibit consistent behavior, with all specimens demonstrating brittle fractures characterized by typical flat cracks upon breaking. A noticeable degradation in mechanical properties is observed with higher AgNP concentrations, although the progression varies.
At a nanoparticle concentration of 5%, the samples exhibit comparable characteristics to the control samples, with no notable distinctions.
However, at concentrations of 10% and 20%, substantial variations in values are apparent, both during traction and at fracture, which are statistically significant when compared to the control samples (Figure 6).
Figure 6.
Tensile strength vs. fracture strength for the two types of resins.

The specimens containing 5% AgNP exhibited mechanical properties closely resembling those of the control group.
Regarding the analysis of surface roughness, the results showed no changes in the roughness of the AgNp-enriched resin surfaces, compared to control samples (Figure 7). It is noted that the inclusion of silver nanoparticles in the composition of acrylic resins does not impact surface conditions and, consequently, does not alter the roughness of the materials. Understanding this fact is crucial as the quality of the complete denture surface is a determinant factor affecting their stability and longevity over time.
Figure 7.
Comparative analysis of roughness values.

Discussion
The materials used in prosthetic constructions undergo changes in their mechanical properties due to various technological processes. Our study explores a conventional method that offers enhanced control over the shape and fit of temporary bridges. Prior research has shown divergent findings concerning the impact of fixed interim restorations on gum health [19]. However, it is commonly believed that well-fitted interim restorations with proper finishing and polishing do not typically lead to gingival inflammation, and our findings support this notion [20].
The concern for optimizing the mechanical properties and biocompatibility of acrylic resins was permanent, but each method had its own drawbacks.
Incorporating AgNPs serves the purpose of reducing microbial colonization or, ideally, preventing it altogether on the acrylic dental resin surfaces. A lot of studies in the field show that silver nanoparticles optimize the biocompatibility of acrylic resins. Researchers have shown that nanoparticles are more effective at increasing the strength of these materials compared to fibers [21,22], and they have concluded that both impact and transverse strengths are increased by the addition of nanoparticles [23,24]. Also important are the size of the nanoparticles and their concentration, as well as the polymerization mechanism [25].
In the literature, there has been a permanent debate regarding the utility of enriching dental materials with nanoparticles; considering the numerous reactions at the level of the oral mucosa in the case of wearers of mobile acrylic prostheses, more and more studies have been carried out regarding the introduction of silver nanoparticles into the structure of these materials, as a solution to these inconveniences.
What concerned the researchers was whether the antibacterial effect of the nanoparticles is counteracted by the modification of the structure and material properties. Sodagar et al. concludes in his research that the effect of AgNPs on the mechanical parameters of PMMA depended on several factors, such as the type of acrylic resin and the concentration of nanoparticles [26].
The study conducted by Chladek et al. highlights the impact of silver nanoparticle concentration on the mechanical and physical properties of the composite. Their findings revealed a decrease in mechanical properties with an increase in silver nanoparticle content. Moreover, research indicates that incorporating metal fillers exceeding 5 wt% into acrylic resin could lead to a reduction in tensile strength [27].
In our study, the results show that there is no significant difference between the parameters of the control samples and the samples enriched with AgNPs at a concentration of 5%. So, temporary bridges made from AgNp-enriched acrylic resin will have optimal mechanical parameters and antibacterial properties, which is a significant advantage in the case of temporary prosthetics for patients with periodontal diseases.
Surface texture has a crucial role in determining the quality of a surface, and it can be evaluated by examining the micrometric profile of finished and polished samples. This texture is quantified by measuring the deviations in the surface’s normal vector from its ideal form. If these deviations are significant, the surface is considered rough; if they are minimal, the surface is deemed smooth. In the field of surface metrology, roughness typically refers to the high-frequency, short-wavelength aspect of a surface profile. However, in practical applications, it is often necessary to consider both the amplitude and frequency to ensure that a surface meets specific requirements. The shape and dimensions of the micrometric profile also has a role in determining how easily bacterial biofilms adhere to and develop on the surfaces of acrylic prostheses. Increased surface roughness promotes plaque retention, facilitating bacterial colonization, particularly along restorative margins, leading to periodontal inflammation and infection. These changes can result in heightened pulpal sensitivity, gingival recession, and tissue inflammation and can pose challenges for restorative rehabilitation efforts. Therefore, achieving an optimal interim restoration quality is essential to mitigate these adverse effects and maintain the integrity of the periodontal restorative interface [28,29,30].
Conclusions
Temporary prosthetic constructions have a crucial role in therapeutic strategies, serving to prevent functional imbalances and the onset of local and loco-regional complications. Various methods and materials can be employed to achieve interim prostheses, depending on their intended purpose and duration of application.
Within the limitation of this study concerning materials for temporary bridges, it can be inferred that incorporating AgNPs at a lower concentration of 5% does not compromise mechanical properties, while simultaneously imparting antibacterial effects. This allows for the fabrication of long-term interim prosthodontic restorations. A higher concentration of nanoparticles may reduce the mechanical properties of resins but does not affect the surface condition of the materials.
Author Contributions
Conceptualization, I.M. and E.C.; Methodology, C.S.; Software, O.M.B.; Validation. D.A.P-D. and C.S.; Formal Analysis, L.P.; Investigation, M.G.N.; Resources, D.A.P-D.; Data Curation, O.M.B.; Writing—Original Draft Preparation, A.J.; Writing—Review and Editing, E.C.; Visualization, C.S.; Supervision, I.M.; Project Administration, D.A.P-D.; Funding Acquisition, I.M. and L.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by The Borrow Foundation, with the research grant being registered at the University of Medicine and Pharmacy “Grigore T. Popa”, Iasi, Romania.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Rayyan, M.M.; Aboushelib, M.; Sayed, N.M.; Ibrahim, A.; Jimbo, R. Comparison of interim restorations fabricated by CAD/CAM with those fabricated manually. J. Prosthet. Dent. 2015, 114, 414–419. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Sayed, M.E.; Shetty, M.; Alqahtani, S.M.; Al Wadei, M.H.D.; Gupta, S.G.; Othma, A.A.A.; Alshehri, A.H.; Alqarni, H.; Mobarki, A.H.; et al. Physical and Mechanical Properties of 3D-Printed Provisional Crowns and Fixed Dental Prosthesis Resins Compared to CAD/CAM Milled and Conventional Provisional Resins: A Systematic Review and Meta-Analysis. Polymers 2022, 14, 2691. [Google Scholar] [CrossRef] [PubMed]
- Benli, M.; Eker-Gümüş, B.; Kahraman, Y.; Huck, O.; Özcan, M. Can polylactic acid be a CAD/CAM material for provisional crown restorations in terms of fit and fracture strength? Dent. Mater. J. 2021, 40, 772–780. [Google Scholar]
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef]
- Mizrah, B. Temporary restaorations the key to succes. Br. Dent. J. 2019, 226, 761–768. [Google Scholar] [CrossRef] [PubMed]
- Tatarciuc, M.; Maftei, G.A.; Vitalariu, A.; Luchian, I.; Martu, I.; Diaconu-Popa, D. Inlay-Retained Dental Bridges—A Finite Element Analysis. Appl. Sci. 2021, 11, 3770. [Google Scholar] [CrossRef]
- Mocanu, R.C.; Martu, M.-A.; Luchian, I.; Sufaru, I.G.; Maftei, G.A.; Ioanid, N.; Martu, S.; Tatarciuc, M. Microbiologic Profiles of Patients with Dental Prosthetic Treatment and Periodontitis before and after Photoactivation Therapy—Randomized Clinical Trial. Microorganisms 2021, 9, 713. [Google Scholar] [CrossRef]
- Hsu, Y.-T.; Huang, N.; Wang, H.-L.; Kuo, Y.-W.; Chen, M.; Liu, T.-K.; Lin, H.-N.; Kuo, S.-L.; Juan, P.-K.; Liao, P.-B. Relationship between periodontics and prosthodontics: The two-way street. J. Prosthodont. Implantol. 2015, 4, 4–11. [Google Scholar]
- Maftei, G.-A.; Martu, M.-A.; Martu, M.-C.; Popescu, D.; Surlin, P.; Tatarciuc, D.; Popa, C.; Foia, L.-G. Correlations between Salivary Immuno-Biochemical Markers and HbA1c in Type 2 Diabetes Subjects before and after Dental Extraction. Antioxidants 2021, 10, 1741. [Google Scholar] [CrossRef]
- Kadiyala, K.K.; Badisa, M.K.; Anne, G.; Anche, S.C.; Chiramana, S.; Muvva, S.B.; Zakkula, S.; Jyothula, R.R.D. Evaluation of Flexural Strength of Thermocycled Interim Resin Materials Used in Prosthetic Rehabilitation—An In-vitro Study. J. Clin. Diagn. Res. 2016, 10, ZC91–ZC95. [Google Scholar] [CrossRef]
- Yanikoğlu, N.D.; Bayindir, F.; Kürklü, D.; Beşir, B. Flexural Strength of Temporary Restorative Materials Stored in Different Solutions. Open J. Stomatol. 2014, 4, 46720. [Google Scholar]
- Aurélio, I.L.; Marchionatti, A.M.E.; Montagner, A.F.; May, L.G.; Soares, F.Z.M. Does air particle abrasion affect the flexural strength and phase transformation of Y-TZP? A systematic review and meta-analysis. Dent. Mater. 2016, 32, 827–845. [Google Scholar] [CrossRef] [PubMed]
- Abad-Coronel, C.; Carrera, E.; Córdova, N.M.; Fajardo, J.I.; Aliaga, P. Comparative Analysis of Fracture Resistance between CAD/CAM Materials for Interim Fixed Prosthesis. Materials 2021, 14, 7791. [Google Scholar] [CrossRef]
- Rosenstiel, S.F.; Land, M.F.; Fujimoto, J. Provisional Restorations in Contemporary Fixed Prosthodontics, 4th ed.; CV Mosby Publishing: St. Louis, MO, USA, 2019; pp. 466–507. [Google Scholar]
- Yin, L.-Z.-X. The Effect of Different Polishing Protocols on Surface Topography and Roughness of Provisional and Semi-PermanentProsthodontic Materials. Dent. Theses 2021, 63, 6–11. [Google Scholar]
- Panáček, A.; Kvítek, L.; Smékalová, M.; Večeřová, R.; Kolář, M.; Röderová, M.; Dyčka, F.; Šebela, M.; Prucek, R.; Tomanec, O.; et al. Bacterial resistance to silver nanoparticles and how to overcome it. Nature Nanotechnology 2018, 13, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Dawadi, S.; Katuwal, S.; Gupta, A.; Lamichhane, U.; Thapa, R.; Jaisi, S.; Lamichhane, G.; Bhattarai, D.P.; Parajul, N. Current Research on Silver Nanoparticles: Synthesis, Characterization, and Applications. J. Nanomater. 2021, 2021, 6687290. [Google Scholar] [CrossRef]
- Mârtu, I.; Murariu, A.; Baciu, E.R.; Savin, C.N.; Foia, I.; Tatarciuc, M.; Diaconu-Popa, D. An Interdisciplinary Study regarding the Characteristics of Dental Resins Used for Temporary Bridges. Medicina 2022, 58, 811. [Google Scholar] [CrossRef]
- Skorulska, A.; Piszko, P.; Rybak, Z.; Szymonowicz, M.; Dobrzyński, M. Review on Polymer, Ceramic and Composite Materials for CAD/CAM Indirect Restorations in Dentistry-Application, Mechanical Characteristics and Comparison. Materials 2021, 14, 1592. [Google Scholar] [CrossRef]
- Al Jabbari, Y.S.; Al-Rasheed, A.; Smith, J.W.; Iacopino, A.M. An indirect technique for assuring simplicity and marginal integrity of provisional restorations during full mouth rehabilitation. Saudi Dent. J. 2013, 25, 39–42. [Google Scholar] [CrossRef]
- Alhawiatan, A.S.; Alqutaym, O.S.; Aldawsari, S.N.; Zuhair, F.A.; Alqahtani, R.O.; Alshehri, T.H. Evaluation of Silver Nanoparticles Incorporated Acrylic Light Cure Resin Trays. J. Pharm. Bioallied Sci. 2020, 12, 173–175. [Google Scholar] [CrossRef]
- Machado, C.; Sanchez, E.; Azer, S.S.; Uribe, J.M. Comparative study of the transverse strength of three denture base materials. J. Dent. 2007, 35, 930–933. [Google Scholar] [CrossRef] [PubMed]
- Bahrani, F.; Safari, A.; Vojdani, M.; Karampoor, G. Comparison of Hardness and Surface Roughness of Two Denture bases Polymerized by Different Methods. World J. Dent. 2012, 3, 171–175. [Google Scholar] [CrossRef]
- Alhareb, A.O.; Akil, H.M.; Ahmad, Z.A. Impact strength, fracture toughness and hardness improvement of PMMA denture base through addition of nitrile rubber/ceramic fillers. Saudi J. Dent. Res. 2017, 8, 26–34. [Google Scholar] [CrossRef]
- Ali, I.L.; Yunus, N.; Abu-Hassan, M.I. Hardness, flexural strength, and flexural modulus comparisons of three differently cured denture base systems. J. Prosthodont. 2008, 17, 545–549. [Google Scholar] [CrossRef]
- Sodagar, J.A.; Kassaee, M.Z.; Akhavan, A.; Javadi, N.; Arab, S.; Kharazifard, M.J. Effect of silver nano particles on flexural strength of acrylic resins. J. Prosthodont. Res. 2012, 56, 120–124. [Google Scholar] [CrossRef]
- Chladek, G.; Kasperski, J.; Barszczewska-Rybarek, I.; Żmudzki, J. Sorption, solubility, bond strength and hardnessof denture soft lining incorporated with silver nanoparticles. Int. J. Mol. Sci. 2013, 14, 563–574. [Google Scholar] [CrossRef]
- Abdullah, A.O.; Pollington, S.; Liu, Y. Comparison between direct chairside and digitally fabricated temporary crowns. Dent. Mater. J. 2018, 37, 957–963. [Google Scholar] [CrossRef]
- Abdulmohsen, B.; Parker, S.; Braden, M.; Patel, M.P. A study to investigate and compare the physicomechanical properties of experimental and commercial temporary crown and bridge materials. Dent. Mater. 2016, 32, 200–210. [Google Scholar] [CrossRef]
- Hahnel, S.; Krifka, S.; Behr, M.; Kolbeck, C.; Lang, R. Performance of resin materials for temporary fixed denture prostheses. J. Oral. Sci. 2019, 61, 270–275. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 Copyright by the authors. Licensed as an open access article using a CC BY 4.0 license.

