Timisoara_Med 2023, 2023(1), 1; doi:10.35995/tmj20230101
Case Report
Assessment of Platelet Mitochondrial Respiration in the Setting of Cardiopulmonary Bypass: A Case Report
1
Doctoral School Medicine-Pharmacy, “Victor Babeș” University of Medicine and Pharmacy of Timișoara, 2 E. Murgu Sq., 300041 Timișoara, Romania; darius.buriman@umft.ro (D.G.B.); braescu.laurentiu@umft.ro (L.A.B.); grigorescu.andrei@umft.ro (A.E.G.)
2
Center for Translational Research and Systems Medicine, “Victor Babeș” University of Medicine and Pharmacy of Timișoara, 2 E. Murgu Sq., 300041 Timișoara, Romania; adimerce@gmail.com (A.P.M.); lungu.anca@umft.ro (A.M.B.); sturza.adrian@umft.ro (A.S.)
3
Institute of Cardiovascular Diseases, 13A Gheorghe Adam Str., 300310 Timișoara, Romania
4
Department of Cardiology – Cardiovascular Surgery, “Victor Babeș” University of Medicine and Pharmacy of Timișoara, E. Murgu Sq., no. 2, 300041 Timișoara, Romania; horea.feier@umft.ro
5
Department of Functional Sciences – Pathophysiology, “Victor Babeș” University of Medicine and Pharmacy of Timișoara, 2 E. Murgu Sq., 300041 Timișoara, Romania
*
Correspondence: daninamuntean@umft.ro
How to cite: Buriman, D.G.; Merce, A.P.; Bînă, A.M.; Brăescu, L.A.; Grigorescu, A.E.; Sturza, A.; Muntean, D.M.; Feier, H.B. Assessment of Platelet Mitochondrial Respiration in the Setting of Cardiopulmonary Bypass: A Case Report. Timisoara Med. 2023, 2023(1), 1; doi:10.35995/tmj20230101.
Received: 21 March 2023 / Accepted: 8 May 2023 / Published: 30 May 2023
Abstract
:Aortic stenosis is the most common valvular disease worldwide. Coronary artery disease (CAD) is often associated with degenerative aortic stenosis, particularly among older patients. Surgical treatment of the combined pathologies is highly recommended because the results are durable. Assessment of mitochondrial respiration in blood cells has recently emerged as a potential biomarker of the bioenergetic health but data regarding the changes in the setting of cardiopulmonary bypass (CPB) are scarce. A 67-year-old man was referred to the clinic for progressive breathlessness, constrictive thoracic pain and fatigue. Investigations revealed severe aortic stenosis and triple-vessel CAD. The aortic valve was replaced with a mechanical aortic prosthesis and coronary artery bypass graft was performed under mild hypothermia. We assessed platelet complex I (CI)- and complex II (CII)-dependent mitochondrial respiration and found a significant increase in the net active respiration supported by CI and the maximal uncoupled respiration in platelets harvested after CPB compared to those isolated pre-CPB. At variance, the active coupled respiration and electron transfer capacity for CII were decreased. The relative contribution of the complex cardiac pathology and CPB to the impairment of CII-dependent respiration and/or a possible relation with patients’ outcome are worth further investigation in a pilot study.
Keywords:
aortic stenosis; bicuspid aortic valve; aortic valve replacement; coronary artery bypass grafting; cardiopulmonary bypass; platelet mitochondrial respirationIntroduction
Calcific aortic stenosis (AS) has been widely reported as the most common valvular heart disease in the ageing population worldwide [1,2]. With the increase in life expectancy of elderly people, particularly in high-income countries, and the strong relationship between AS and age, it has been predicted that the prevalence of the disease will double in the coming decades [3]. AS is characterized by obstruction to left ventricular (LV) outflow, determined by progressive fibro-calcific remodeling and thickening of the aortic valve leaflets [4]. Once diagnosed, the progression is inevitable and the disease has a poor prognosis in symptomatic patients [5].
The bicuspid aortic valve (BAV) represents the most frequent congenital cardiovascular malformation, with a prevalence of 2.25% in the general population [6]. Congenital abnormality (bicuspid aortic valve) and older age are powerful risk factors for calcific AS [7]. Patients with congenital bicuspid AS are four times more likely to be male and present with severe calcific AS after the age of 50. Bicuspid AS is thought to clinically manifest approximately two decades earlier than tricuspid AS because of increased leaflet stress and turbulent flow attributed to the abnormal architecture of the aortic valve [8].
Regardless the etiology, advanced AS features an active process of extensive extracellular matrix remodeling, valvular fibrosis and calcification. Currently, there is no successful pharmacological treatment available to prevent or slow its progression and aortic valve replacement (AVR) remains the only effective treatment for severe AS. International guidelines recommend surgical replacement in BAV patients, despite the increasing use of the less invasive and more attractive transcatheter therapy in the elderly population. There is an unmet need for studies assessing the long-term outcomes and valve performance in AS patients with an indication for surgery due to BAV. This is particularly true when considering the fact that BAV patients are at a higher risk for developing bicuspid aortopathy, a condition characterized by aortic dilatation and potential life-threatening complications such as aortic dissection or aortic root aneurysm with rupture [9,10,11].
Calcified aortic stenosis is frequently associated with coronary arteries disease (CAD) and coronary artery bypass (CABG) is required to be performed during the AVR procedure [8]. Nowadays, the current understanding of the disease postulates that an intricate and progressive process of active valvular and vascular calcification occurs potentiated by age- and stress-induced cellular senescence [12].
In an attempt to provide a risk stratification of the disease, over the last decade, several biomarkers have been investigated in AS patients. Among the blood biomarkers, a number of studies have demonstrated the usefulness of high-sensitivity cardiac troponin, lipoprotein (a), and brain natriuretic peptides (recently reviewed in ref. [13]).
Platelet mitochondrial respiration has recently emerged as a potential biomarker for the assessment of the bioenergetic status in both acute and chronic pathologies [14]. However, literature regarding the effects of CPB on platelet respiration is scarce. In a pioneering study, Mazzeffi et al. reported that “typical” CPB durations of 1.5 to 3 hours elicited no significant effect on platelet mitochondrial respiration at the end of the procedure, as assessed using the XF24e Extracellular Flux Analyzer (Seahorse-Agilent) [15].
Here, we present a case of severe aortic stenosis and multiple vessel coronary artery disease who underwent elective surgery for both pathologies, and in which mitochondrial respiration was assessed in platelets harvested both prior and after cardiopulmonary bypass (CPB) by means of the high-resolution respirometry (HRR) technique using the O2k Oxygraph (Oroboros Instr.)
Case Report
We present the case of a 67-year-old male patient, diagnosed with severe aortic stenosis on a bicuspid aortic valve (BAV) and severe coronary artery disease. The patient was admitted complaining of progressive breathlessness, constrictive thoracic pain and fatigue. The physical examination revealed peripheral edema, while cardiovascular examination found a systolic crescendo–decrescendo murmur, heard loudest at the right upper sternal border and a delayed second heart sound (S2). The chest X-ray exam identified prominent broncho-vascular markings with normal heart size.
Blood pressure at arrival was 128/75 mmHg. The ECG at admission showed sinus rhythm, and an HR of 75 bpm. Standard blood tests were within the normal limits, but the HCV antibody test was positive.
Transthoracic echocardiography revealed the following findings: a normal left ventricular size and function, with an ejection fraction of 50–55%, a bicuspid aortic valve with severe stenosis (mean gradient, 53 mmHg; aortic valve area, 0.8 cm2), and the right coronary cusp fused with the non-coronary cusp. There was also ultrasound evidence for mild aortic regurgitation, mild mitral regurgitation, mild secondary pulmonary hypertension but with normal right ventricle size and systolic function.
Coronary angiography showed: an 80% stenosis in segment III of the right coronary artery, chronic proximal occlusion of the circumflex artery, retrogradely perfused through the collaterals, ostial stenosis and 80–90% stenosis in segment II of the left anterior descending coronary artery (Figure 1).
The patient was operated by midline sternotomy and was cannulated via the aorta and the venous canulation was performed via a double stage venous canula inserted in the right atrial appendage. The patient was placed on cardiopulmonary bypass and cooled to 34 °C. A left ventricular vent was placed via the right superior pulmonary vein to maintain a dry operative field. An aortic root cannula was placed in the ascending aorta for the antegrade cardioplegia. Flow into the cardioplegic circuit consisted of cold blood and St. Thomas Hospital cardioplegic solution administered antegrade with additional doses of cardioplegia (5 mL/kg) given approximately every 15–20 minutes throughout the remainder of the cross-clamp period. Distal anastomoses were firstly performed after preparation of the saphenous veins for anastomosis (Figure 2).
A transverse aortotomy was performed approximately 1 cm above the right coronary artery take-off, slightly above the level of the sino-tubular ridge. The incision was extended three-quarters of the way around the aorta. The leaflets of the aortic valve were excised to the level of the annulus and the annulus was thoroughly debrided of calcium deposits. Sutures with pledgets (16 Ti Chron 2-0) and a mechanical aortic prosthesis (23 mm) were utilized (Figure 3).
After valve replacement, the distal anastomosis of the left internal mammary artery to the left anterior descending coronary artery was performed. Finally, the proximal anastomoses of saphenous veins to the ascending aorta were performed. CPB was gradually and uneventfully stopped. The patient was extubated the following day and had an uneventful recovery. No blood derivatives were administered during the surgical procedure, thus platelet harvesting pre-CPB (i.e., prior to the administration of heparin) and post-CPB (within 10 min after the administration of protamine sulphate) was not influenced. Postoperative echocardiography revealed normal function for the aortic mechanical prosthesis, and normal left ventricular size and function (ejection fraction, 50–55%).
Experimental Protocols
Platelet Isolation
The study protocol was approved by the Commitee for Research Ethics of the “Victor Babeș” University of Medicine and Pharmacy from Timișoara, Romania (no. 04p/17/12/2020) and explained to the patient, who signed the written informed consent prior to surgery. The platelet suspension was prepared from 20 mL of peripheral blood collected in K2(EDTA) tubes before and after CPB. A two-step centrifugation (10 min at 500× g, and 5 min at 4600× g) was performed at room temperature, as described in ref. [16]. Platelets were collected in approx. 1 mL of autologous plasma and further used for high-resolution respirometry (HRR) studies at 37 °C, with the Oxygraph-2k (Oroboros Instr., Innsbruck, Austria) according to a protocol detailed in ref. [17]. Before each experiment air calibration was conducted.
Platelet High-Resolution Respirometry
Platelets (2 × 108 cells/chamber) were loaded in each of the two chambers of the O2K oxygraph in MiR05 respiration buffer (with a standard composition: EGTA 0.5 mM, taurine 20 mM, sucrose 110 mM, HEPES 20 mM, MgCl2 · 6 H2O 3 mM, KH2PO4 10 mM, K-lactobionate 60 mM, bovine serum albumin/ BSA 1 g/L, pH 7.1). A protocol using a titration sequence for substrate–uncoupler–inhibitor was adapted to measure complex I (CI)- and complex II (CII)-supported platelet respiration. The main respiratory parameters were as follows: ROUTINE respiration (respiration based on endogenous substrates), OXPHOS capacity or the maximal coupled respiration (corresponding to the active oxidative phosphorylation stimulated by saturating ADP and substrate concentrations for CI and CII), LEAK or the non-phosphorylating respiration (corresponding to the oxygen consumption used to restore the dissipative proton leak elicited in the presence of oligomycin), and ET capacity or the maximal uncoupled respiration (corresponding to the electron transport system capacity through CI and CII, in the presence of an uncoupling agent, e.g., p-trifluoromethoxyphenylhydrazone or FCCP).
After platelet loading, cellular respiration was allowed to stabilize at a steady-state for approx. 15 min in order to measure the ROUTINE respiration (i.e., the respiration in the physiological coupling state). The addition of substrates and modulators of mitochondrial respiration started after plasma membrane permeabilization with digitonin (to allow the substrates to enter the platelets) with the preservation of the intracellular organelles (mitochondria and endoplasmic reticulum) membrane integrity.
CI-supported OXPHOS was measured in the presence of malate (5 mM), glutamate (5 mM), and ADP (1 mM). Succinate (10 mM) was further added to induce maximal respiratory capacity (i.e., CI- and CII-supported OXPHOS). In HRR experiments, the addition of conventional substrates for CI and CII and the subsequent convergent electron flow into the Q-junction was used to mimic an operating Krebs cycle in the intact cell (i.e., with the generation of NADH and succinate in the mitochondrial matrix).
LEAK respiration, a proxy for the passive proton leak, is induced in HRR experiments by inhibiting the phosphorylation pathway with oligomycin (1 μg/mL), thus allowing the measurement of non-phosphorylating respiration.
ET capacity (CI+CII) was further obtained by stepwise titrations (6 μM/step) with the protonophore FCCP until the detection of the highest respiratory flux, which indicates the maximal non-coupled respiration. Complex I activity was then inhibited by rotenone (2 μM), thus allowing the CII-supported ET capacity to be assessed. Inhibition of complex III activity using antimycin A (1 μg/mL) resulted in very slow rates of O2 consumption known as the residual oxygen consumption (ROX) due to processes other than oxidative phosphorylation; the latter values were subtracted from all respiratory rates. DatLab7 software of the Oxygraph-2k was used to record the oxygen concentration and oxygen consumption rate (flux) in real-time.
Results
The results of the HRR experiments performed pre- and post-CPB are summarized in Table 1.
As shown in Table 1, a significant increase in CI-supported OXPHOS (71.36%) was observed in platelets isolated post-CPB vs. pre-CPB in contrast to the minor increase in maximal active respiration when succinate, the CII substrate, was further added to the chamber (22.13%).
Net OXPHOS and ET capacity were obtained by correcting the OXPHOS and ET values for the LEAK values, computed as follows: OXPHOSCI+CII – LEAK and ET capacity – LEAK, respectively.
The ET reserve capacity was calculated by subtracting the ROUTINE values from the ET capacity values (ET capacity – ROUTINE).
Net OXPHOS capacity, an index of ADP stimulation, showed an important increase of 76.67% in platelets harvested post-CPB compared to pre-CPB values. A similar result was found for the net ET capacity, i.e., an increase of 62.63%, at the end of the procedure. However, the ET reserve capacity that indicates the potential of substrate uptake was only mildly increased post-CPB (18.29%).
LEAK, the mitochondrial respiration when ADP has been phosphorylated to ATP, is a measure of the non-phosphorylating respiration and was decreased post-CPB with 27.93%. A similar decrease (28.49% vs. pre-CPB) was found for the ET capacity supported by complex II.
Discussion
The bicuspid aortic valve (BAV) represents the most frequent congenital cardiovascular malformation, which typically presents with severe calcific aortic stenosis after the 50 years.
The current understanding the AS pathophysiology postulates that the disease is an active, evolving process rather than a passive, degenerative entity [1]. Calcified aortic stenosis is frequently associated with CAD and share, at least in part, common pathophysiological features. The current paradigm postulates that BAV evolves in two phases: (i) the early one, when the risk factors (dyslipidemia, hypertension, obesity, high Lp(a) levels, smoking, etc.) and the events (increased expression of adhesion molecules, subendothelial lipoprotein accumulation and oxidation, activation of inflammation, shear stress, etc.) are common with atherosclerosis, and (ii) the late stage, when leaflet fibrosis and calcification leading to progressive valve stiffness are dominant. Increased afterload due to valve obstruction elicits a hypertrophic compensatory response in the left ventricle which restores wall stress and maintains cardiac performance for decades [3]. In time, decompensation and transition to heart failure occur, which in our patient was with preserved EF. In patients with BAV and severe CAD, CABG is indicated to be performed during the same surgical intervention for valve replacement; sudden death from AS with the onset of symptoms is 25% per year without surgical intervention [18].
During open heart surgery, two events mediate cardiac damage: the exclusion of the heart from systemic circulation, which renders the myocardium ischemic and causes reperfusion injury upon blood flow restoration. In myocardial ischemia–reperfusion injury, mitochondria are considered the final effectors responsible for the extent of mitochondrial damage and also the targets of cardioprotective strategies [19]. Cherry has recently reviewed the cardiac mitochondrial dysfunction in cardiac surgery, stating that various factors during the surgical period, such as ischemia–reperfusion injury and increased systemic inflammation from exposure to CPB and surgical trauma, can affect mitochondrial function. Individuals with pre-existing conditions, such as diabetes, heart failure, advanced age, or cardiomyopathies, may have weakened mitochondrial function or be more susceptible to perioperative injury. Hypothermia, on the other hand, can reduce the impact of CPB on mitochondrial function [20]. Of note, this patient underwent mild hypothermia (34 °C for 90 min) during the procedure.
In a patient with chronic cardiac pathology we reported post-CPB a minor increase in the active coupled respiration (OXPHOS) supported by complex II together with a decrease in the maximal non-coupled respiration for CII. These changes may be the result of the: (i) inhibition of substrate (succinate) transport across the mitochondrial inner membrane, (ii) damage to CII within the electron transport system, or (iii) reduced activity of a rate-controlling enzyme in the citric acid cycle.
We have previously demonstrated that a mitochondriotropic drug, NV118 belonging to the class of membrane permeable succinates, is able to improve mitochondrial respiratory function when acutely incubated ex vivo with platelets isolated both pre- and post-CPB. The finding that a membrane-permeable succinate was able to increase oxygen consumption suggests that platelet oxidative metabolism is limited by the concentration of succinate as an energetic substrate [16].
Further experiments are required to elucidate how limitation of the oxidative metabolism by succinate as an energetic substrate and/or an early impairment of CII relate to the chronic cardiovascular pathology and CPB procedure.
Conclusions
This case is worth mentioning as a starting point for prospective studies aimed at characterizing the mitochondrial respiratory dysfunction in blood cells harvested from cardiac patients with the indication of open heart surgery and cardiopulmonary bypass. Whether the above-described changes in platelet respiration can be recapitulated in a proof-of-concept study in patients with various cardiac pathologies and correlate with the exposure to hypothermia and/or the inflammatory status remain to be determined.
Author Contributions
Conceptualization, D.G.B., D.M.M., H.B.F.; methodology, A.P.M., A.M.B., L.A.B., A.E.G.; writing—original draft preparation, D.G.B., A.M.B.; visualization A.S.; writing—review and editing, supervision D.M.M., H.B.F. All authors contributed to the article and approved the submitted version.
Institutional Review Board Statement
The study protocol and informed consent were approved by the Commitee for Research Ethics of “Victor Babeș” University of Medicine and Pharmacy of Timisoara, Romania (No. 04p/17.12.2020).
Acknowledgments
We acknowledge the expert technical assistance of Andreea Anechitei.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kodra, A.; Kim, M. Calcific Aortic Valve Stenosis with Aging and Current Development in its Pathophysiology. Int. J. Angiol. 2022, 31, 229–231. [Google Scholar] [CrossRef] [PubMed]
- Yadgir, S.; Johnson, C.O.; Aboyans, V.; Adebayo, O.M.; Adedoyin, R.A.; Afarideh, M.; Alahdab, F.; Alashi, A.; Alipour, V.; Arabloo, J.; et al. Global, Regional, and National Burden of Calcific Aortic Valve and Degenerative Mitral Valve Diseases, 1990–2017. Circulation 2020, 141, 1670–1680. [Google Scholar] [CrossRef] [PubMed]
- Lindman, B.R.; Sukul, D.; Dweck, M.R.; Madhavan, M.V.; Arsenault, B.J.; Coylewright, M.; Merryman, W.D.; Newby, D.E.; Lewis, J.; Harrell, F.E., Jr.; et al. Evaluating Medical Therapy for Calcific Aortic Stenosis: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2021, 78, 2354–2376. [Google Scholar] [CrossRef]
- Goody, P.R.; Hosen, M.R.; Christmann, D.; Niepmann, S.T.; Zietzer, A.; Adam, M.; Bönner, F.; Zimmer, S.; Nickenig, G.; Jansen, F. Aortic Valve Stenosis: From Basic Mechanisms to Novel Therapeutic Targets. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 885–900. [Google Scholar] [CrossRef]
- Peeters, F.; Meex, S.J.R.; Dweck, M.R.; Aikawa, E.; Crijns, H.; Schurgers, L.J.; Kietselaer, B. Calcific aortic valve stenosis: Hard disease in the heart: A biomolecular approach towards diagnosis and treatment. Eur. Heart J. 2018, 39, 2618–2624. [Google Scholar] [CrossRef] [PubMed]
- Perrin, N.; Ibrahim, R.; Dürrleman, N.; Basmadjian, A.; Leroux, L.; Demers, P.; Modine, T.; Ben Ali, W. Bicuspid Aortic Valve Stenosis: From Pathophysiological Mechanism, Imaging Diagnosis, to Clinical Treatment Methods. Front. Cardiovasc. Med. 2021, 8, 798949. [Google Scholar] [CrossRef] [PubMed]
- Engel Gonzalez, P.; Kumbhani, D.J. Treatment of Bicuspid Aortic Valve Stenosis Using Transcatheter Heart Valves. Interv. Cardiol. Clin. 2021, 10, 541–552. [Google Scholar] [CrossRef] [PubMed]
- Boskovski, M.T.; Gleason, T.G. Current Therapeutic Options in Aortic Stenosis. Circ. Res. 2021, 128, 1398–1417. [Google Scholar] [CrossRef] [PubMed]
- Nappi, F.; Giacinto, O.; Lusini, M.; Garo, M.; Caponio, C.; Nenna, A.; Nappi, P.; Rousseau, J.; Spadaccio, C.; Chello, M. Patients with Bicuspid Aortopathy and Aortic Dilatation. J. Clin. Med. 2022, 11, 6002. [Google Scholar] [CrossRef] [PubMed]
- Fatehi Hassanabad, A.; King, M.A.; Di Martino, E.; Fedak, P.W.M.; Garcia, J. Clinical implications of the biomechanics of bicuspid aortic valve and bicuspid aortopathy. Front. Cardiovasc. Med. 2022, 9, 922353. [Google Scholar] [CrossRef] [PubMed]
- Yassine, N.M.; Shahram, J.T.; Body, S.C. Pathogenic Mechanisms of Bicuspid Aortic Valve Aortopathy. Front. Physiol. 2017, 8, 687. [Google Scholar] [CrossRef] [PubMed]
- Molnár, A.; Pásztor, D.; Merkely, B. Cellular Senescence, Aging and Non-Aging Processes in Calcified Aortic Valve Stenosis: From Bench-Side to Bedside. Cells 2022, 11, 3389. [Google Scholar] [CrossRef] [PubMed]
- Shen, M.; Tastet, L.; Bergler-Klein, J.; Pibarot, P.; Clavel, M.A. Blood, tissue and imaging biomarkers in calcific aortic valve stenosis: Past, present and future. Curr. Opin. Cardiol. 2018, 33, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Petrus, A.T.; Lighezan, D.L.; Danila, M.D.; Duicu, O.M.; Sturza, A.; Muntean, D.M.; Ionita, I. Assessment of platelet respiration as emerging biomarker of disease. Physiol. Res. 2019, 68, 347–363. [Google Scholar] [CrossRef] [PubMed]
- Mazzeffi, M.; Lund, L.; Wallace, K.; Herrera, A.V.; Tanaka, K.; Odonkor, P.; Strauss, E.; Rock, P.; Fiskum, G. Effect of cardiopulmonary bypass on platelet mitochondrial respiration and correlation with aggregation and bleeding: A pilot study. Perfusion 2016, 31, 508–515. [Google Scholar] [CrossRef] [PubMed]
- Merce, A.P.M.; Bînă, A.M.B.; Avram, V.F.A.; Buriman, D.G.B.; Lascu, A.L.; Feier, H.B.F.; Petrescu, L.P.; Muntean, D.M.M.; Elmér, E.E.; Crețu, O.M.C. Cell-Permeable Succinate Improves Platelet Respiration in Patients Undergoing Cardiopulmonary Bypass: A Pilot Study. Timisoara Med. J. 2022, 2022, 2. [Google Scholar]
- Bînă, A.M.; Aburel, O.M.; Avram, V.F.; Lelcu, T.; Lința, A.V.; Chiriac, D.V.; Mocanu, A.G.; Bernad, E.; Borza, C.; Craina, M.L.; et al. Impairment of mitochondrial respiration in platelets and placentas: a pilot study in preeclamptic pregnancies. Mol. Cell. Biochem. 2022, 477, 1987–2000. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. J. Cardiothorac. Surg. 2021, 60, 727–800. [Google Scholar] [CrossRef] [PubMed]
- Niemann, B.; Schwarzer, M.; Rohrbach, S. Heart and Mitochondria: Pathophysiology and Implications for Cardiac Surgeons. Thorac. Cardiovasc. Surg. 2018, 66, 11–19. [Google Scholar] [CrossRef]
- Cherry, A.D. Mitochondrial Dysfunction in Cardiac Surgery. Anesthesiol. Clin. 2019, 37, 769–785. [Google Scholar] [CrossRef] [PubMed]
Figure 1.
Coronary angiography. An 80% stenosis in segment III of the right coronary artery (A). Proximal occlusion of the circumflex artery (B). Ostial stenosis and 80–90% stenosis in segment II of the left anterior descending coronary artery (C).
Figure 1.
Coronary angiography. An 80% stenosis in segment III of the right coronary artery (A). Proximal occlusion of the circumflex artery (B). Ostial stenosis and 80–90% stenosis in segment II of the left anterior descending coronary artery (C).

Figure 2.
Preparation of the saphenous vein for anastomosis (upper panel). Distal anastomosis of the saphenous vein graft to left circumflex artery (lower panel).
Figure 2.
Preparation of the saphenous vein for anastomosis (upper panel). Distal anastomosis of the saphenous vein graft to left circumflex artery (lower panel).

Figure 3.
Mechanical aortic valve prosthesis nr. 23 mm.
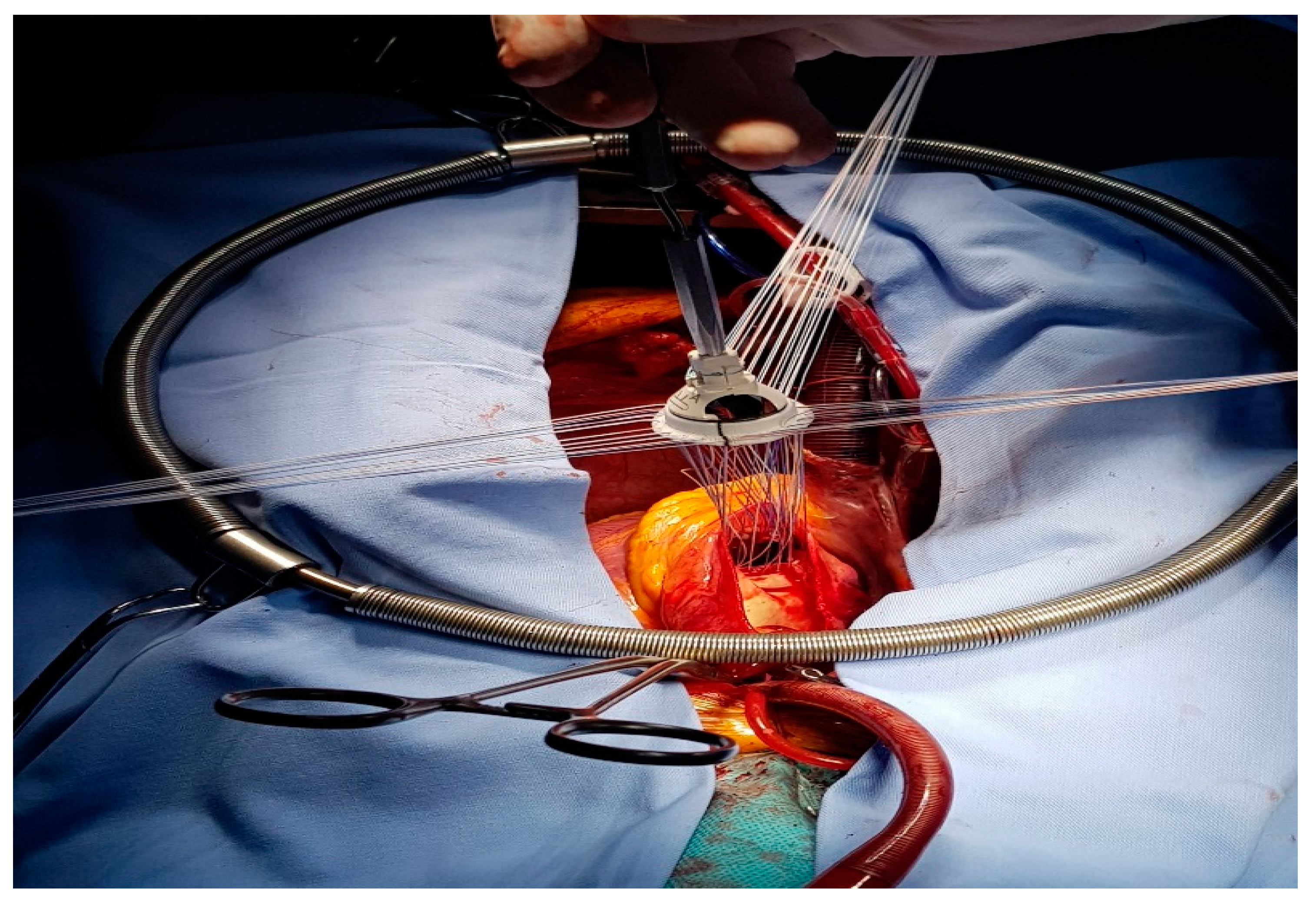
Table 1.
Mitochondrial respiratory parameters assessed by HRR in platelets isolated pre- and post-CPB.
Table 1.
Mitochondrial respiratory parameters assessed by HRR in platelets isolated pre- and post-CPB.
| Respiratory States in Permeabilized Platelets | PRE-CPB (pmol O2 × s−1 × 2 × 108 Cells) | POST-CPB (pmol O2 × s−1 × 2 ×108 Cells) | Percentage Change |
|---|---|---|---|
| ROUTINE | 13.85 | 16.82 | ↑ 21.44% |
| OXPHOS CI | 15.96 | 27.35 | ↑ 71.36% |
| OXPHOS CI+CII | 26.97 | 32.94 | ↑ 22.13% |
| LEAK | 14.93 | 11.67 | ↓ 27.93% |
| ET CAPACITY | 29.43 | 35.25 | ↑ 19.77% |
| ETCII | 20.43 | 15.9 | ↓ 28.49% |
| NET OXPHOS | 12.04 | 21.27 | ↑ 76.67% |
| NET ET CAPACITY | 14.5 | 23.58 | ↑ 62.63% |
| ET-RESERVE CAPACITY | 15.58 | 18.43 | ↑ 18.29% |
CPB: cardiopulmonary bypass; ROUTINE: respiration supported by endogenous substrates and ADP; OXPHOSCI: complex I-supported oxidative phosphorylation; OXPHOSCI+CII: complex I- and II-supported oxidative phosphorylation (maximal coupled respiration); LEAK: non-phosphorylating respiration; ET capacity: maximal electron transport capacity supported by complex I and II (maximal non-coupled respiration); ETCII: maximal electron transport capacity supported by complex II.
© 2023 Copyright by the authors. Licensed as an open access article using a CC BY 4.0 license.


